Short Bowel Syndrome in Children
Most children with SBS develop the condition shortly after birth due to an underlying gastrointestinal (GI) condition, leading to intestinal surgery. Their journey can differ from that of adults.
Short bowel syndrome (SBS) is a serious and chronic malabsorption disorder.
SBS occurs when parts of the intestine are removed surgically and the remaining intestine may not be able to absorb enough nutrients from food and drink.
This results in malabsorption. It puts people at risk for:

Malnutrition

Electrolyte disturbances

Dehydration

Diarrhea/increased outputs
Some children with SBS will be able to eat and drink, and some will require additional support from one of the following methods.
enteral nutrition
Feeding through a tube linked to the stomach or small intestine.

parenteral support (also known as PS)

Feeding through a vein to the bloodstream, and can range from fluids and electrolytes to a complete mix of nutrients.
A type of PS that provides all of the child’s nutritional needs is known as total parenteral nutrition (TPN).
The total number of children with SBS appears to be increasing as more newborns survive the genetic or birth conditions that can lead to bowel resection surgery.
Since SBS in children is so rare, it is difficult to estimate how many children have it.
Signs and Symptoms of SBS in children
Malabsorption
Growth and developmental delays
Fluid, electrolyte, micronutrient deficiency
Diaper/stoma skin breakdown
Bone density issues/fractures
Lactic acid buildup
Kidney stones
Motility disturbances
Heartburn
Ulcers
Gallstones
If your child does not have an SBS diagnosis but is exhibiting any of these symptoms (or a combination) following a bowel resection, it is a good idea to talk to your doctor.
This guide may help.
Doctor Discussion GuideWhat Conditions May Lead to Short Bowel Syndrome in Children?
In children, SBS usually results from problems at birth
There are other causes, but the majority of SBS cases stem from genetic or birth conditions that can lead to bowel resection surgery.
Necrotizing enterocolitis, commonly referred to as NEC, is the most common cause of SBS in infants. NEC usually happens in premature infants, and occurs when the lining of the intestinal wall dies. NEC generally occurs in the first 2 weeks after a child has been introduced to oral feedings.
IA, or intestinal atresia, occurs in infants who haven’t formed their intestines completely. Instead of their bowels acting like an open tube, they are closed off in 1 or more places, which can cause blockage or obstruction and infection.
This condition occurs when an infant’s intestines develop outside of the body through a hole in the abdominal wall. Since the intestines aren’t protected, the bowels can become irritated, injured, or prone to infection.
Volvulus is a twisting of the intestine that can cause a blockage and cut off blood flow. The damaged tissue, starved of oxygen, may need to be removed via resection. Malrotation occurs at birth when the intestine fails to rotate fully into its normal position.
This is a disorder caused when an infant is missing certain kinds of nerves in a segment of the intestine. These nerves control peristalsis, which is the movement that muscles make in the bowel to push food through the digestive tract. The inability to have effective bowel movements can lead to constipation or bowel obstruction.
Other conditions may include trauma to the intestines (from an accident, for example).
SBS Management in Children
Considerations for managing SBS in children
SBS results from the body’s inability to absorb enough nutrition from food and drinks.
There are 3 important goals to keep in mind for children with SBS:

Optimize nutrition for normal growth and development

Promote intestinal adaptation

Reduce or eliminate parenteral support
For children with SBS, the first concern in managing SBS is making sure they receive the right nutrition to help ensure that they meet important growth and developmental milestones. Parenteral support, also known as PS, refers to feeding intravenously, and can range from fluids and electrolytes to a complete mix of nutrients.
Expectations following bowel resection
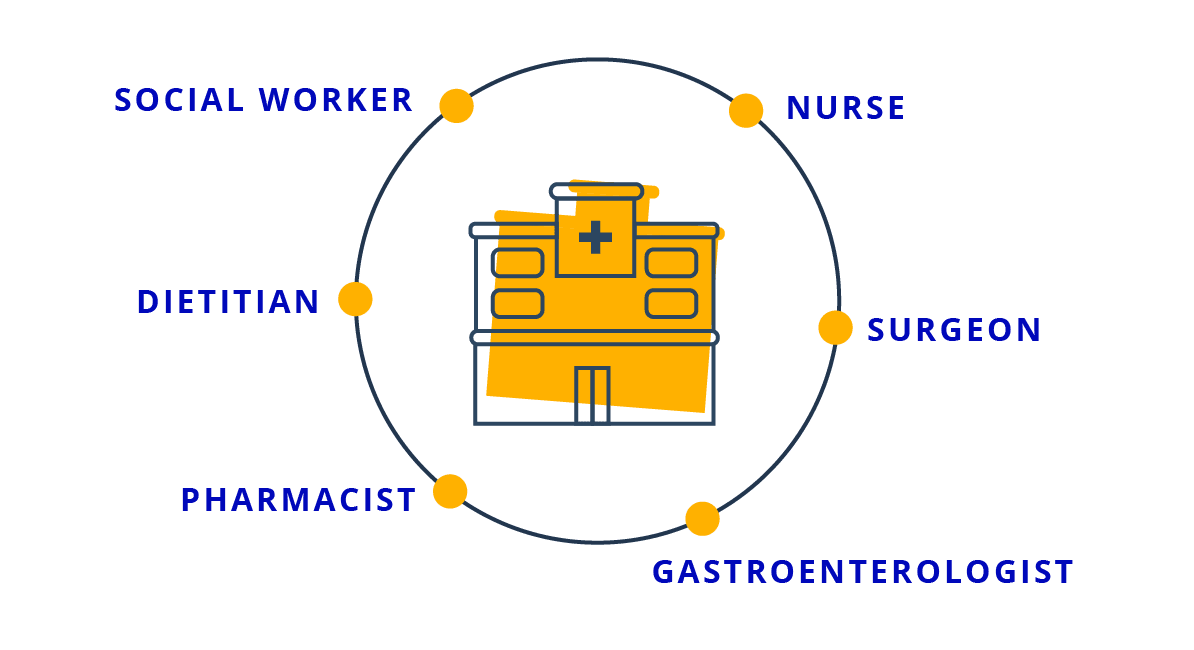
Intestinal resection is serious, but over time survival in newborns is improving. There is evidence that having a multidisciplinary team of healthcare providers improves outcomes, including babies who were unable to wean off parenteral support completely.
Having different specialties involved in your child’s care promotes better coordination of their surgical, medical, and nutritional management. It can lead to a more integrated care plan, better maintenance of medication, and robust communication between providers and family.
The Care Team May Include

Dietitian
Nurse
Surgeon
Social Worker
Pharmacist
Gastroenterologist
Yes, he’s doing great. Yes, he’s thriving. But yes, he will always have short bowel syndrome."


Following surgery, introducing nutrition through a gastrostomy tube, or G-tube, directly to the GI tract as early as possible is important. Tube feeds are usually given slowly over a long period of time to maximize absorption. Continuous tube feeding enhances adaptation and weight gain, which can allow babies to reduce their dependency on parenteral support.
Children should begin having age-appropriate food (for example, breast milk or formula) by mouth as soon as it can be tolerated. Oral feeding helps prevent eating disorders from developing later on.
Transitions of Care are the key milestones a patient with short bowel syndrome may experience. For a child with SBS, medical care changes as the patient grows, and so do the child’s needs, resources, and support. The Transitions of Care Guide can help increase awareness of these important transitions.
To learn more about managing SBS in children, sign up to receive a free copy of “A Kid’s Guide to Short Bowel Syndrome,” by Tegan Medico, MS, RDN, CNSC & Carol Rees Parrish, MS, RD.
Reducing parenteral support through improved intestinal adaptation
Early on, parenteral support is lifesaving for children with SBS and is considered the standard of care. However, the long-term impact of parenteral support can be an important concern.
Children who depend on parenteral support over the long term are prone to life-threatening complications, such as:

LIVER DISEASE
which can have multiple causes, including the delivery of high sugar, protein, and fat into the blood

INFECTIONS
that can lead to organ failure (sepsis)

BLOOD CLOTS
which can prevent the blood from flowing normally

FLUID AND ELECTROLYTE IMBALANCES
Furthermore, parenteral support does not help the intestine improve its ability to absorb food and drink naturally. Successful adaptation allows children to grow and remain healthy.
For many children with SBS, intestinal adaptation is the body’s natural response to a shorter intestinal system. Through this process, the remaining bowel can change its structure and function to be able to help the body absorb the nutrients it needs.
In one US study, almost half of babies with SBS were able to stop parenteral support over their first 5 years after birth. Some children did return to IV nutrition temporarily before regaining independence.*
*The information for this study was collected from 272 babies from the years 2000 to 2007.
Surgical solutions or prescription medicines may help some children achieve independence from PS. Decisions about the appropriate path for your child should be made in consultation with their healthcare team.
Life with nutritional support
Parenteral support will likely be used for some period of time following your child’s surgery. Even children who weaned off nutritional support early often need to go back on IV nutrition later on. Rapid growth spurts at puberty or adolescence can surpass the body’s ability to provide sufficient nutrients.
Transitioning from parenteral support to enteral nutrition, which may be a mix of tube feeding and oral intake, can take a year or longer when it is possible. It is common for this process to take 3 or 4 years. Even after a child has completely weaned off parenteral support, they remain at risk for nutrient deficiencies, such as vitamins or iron. Therefore, it is important to monitor them regularly in case specific supplements are needed in their diet.

No matter the type of nutritional support your child requires, help is available.
Here are some general tips for adjusting to life with a loved one on nutritional support:
- If your child relies on nutritional support at home, a nurse or representative from the home care agency should show you what equipment to use and how to use it.
- Remember to ask questions and even take notes when he or she is giving you this information.
- Don’t be afraid to speak up or ask for additional help if you’re not comfortable with the equipment.
LOOKING TO THE FUTURE
Hope for independence
Thanks to progress in SBS treatment and management, the future holds hope for many children as they grow up. Celia was diagnosed with SBS as a child, and is a successful college student.

“My life with short bowel syndrome looks a lot like someone who doesn’t have short bowel syndrome. I eat…I go to concerts with friends, I go to parties with my family.”
Celia, diagnosed with SBS shortly after birth
Coping with emotional challenges
CHILDREN WITH SBS
For children with SBS, daily life can be an emotional challenge as well as a physical one. The feelings of being different, the frustrations of managing nutritional needs, worrying about where the nearest bathroom is—all of these things can add an emotional burden. As children grow, they may also become increasingly conscious of how others perceive them, which can cause additional stress.
CAREGIVERS
Caregivers, too, face their own challenges, including difficulty in getting a full night’s sleep. It’s so important that caregivers of children with SBS seek support and resources wherever they can find them. Our caregiver resources are a good place to start.
View Advocacy GroupsIf you are a caregiver of a child with SBS, it may be valuable to talk with your healthcare team about whether counseling would be helpful for your child. There are also organizations where you can talk with other parents about the strategies and resources they rely upon to help their children cope.
There are going to be hard days, but just try not to rush the process. Know that the tough moments will not last forever.”

Our SBS Facebook community is a helpful resource to connect with others who are raising a child with SBS
Growing Up
As children with SBS grow up, it’s essential to consider their changing needs to make sure they stay healthy and are prepared for a life with SBS.

ENTERING ADOLESCENCE
This is an important time for children who are reliant on parenteral support to learn the considerations and techniques necessary for managing the parenteral nutrition system. This includes making sure they know how to keep their central line clean and clear, paying attention to hydration, and being prepared for medical emergencies.
Early and repeated practice with their equipment can help children better learn to manage and care for it sooner, while also helping them to gain independence.

THE TEEN YEARS
As children with SBS become adolescents and start college, they and their caregivers should start talking to their healthcare team as early as possible about making a smooth transition from their pediatrician or pediatric gastroenterologist to a team experienced in treating adults.

PREPARING FOR ADULT INDEPENDENCE
In the years leading up to adulthood, it’s a good idea to talk with your current healthcare provider and insurance carrier for recommendations to ensure a seamless transition. Others with SBS who have made this transition may also have helpful guidance and learnings to share—connect with them in our SBS Facebook community.
SBS is serious and requires awareness, attention, and management.
When caregivers, families, and a healthcare team are actively involved, it can set a child with SBS up for success. Each child develops at a different rate, and their readiness for these transitions may be different from another child with SBS.
Learn more with SBS resources and find support.